Shock
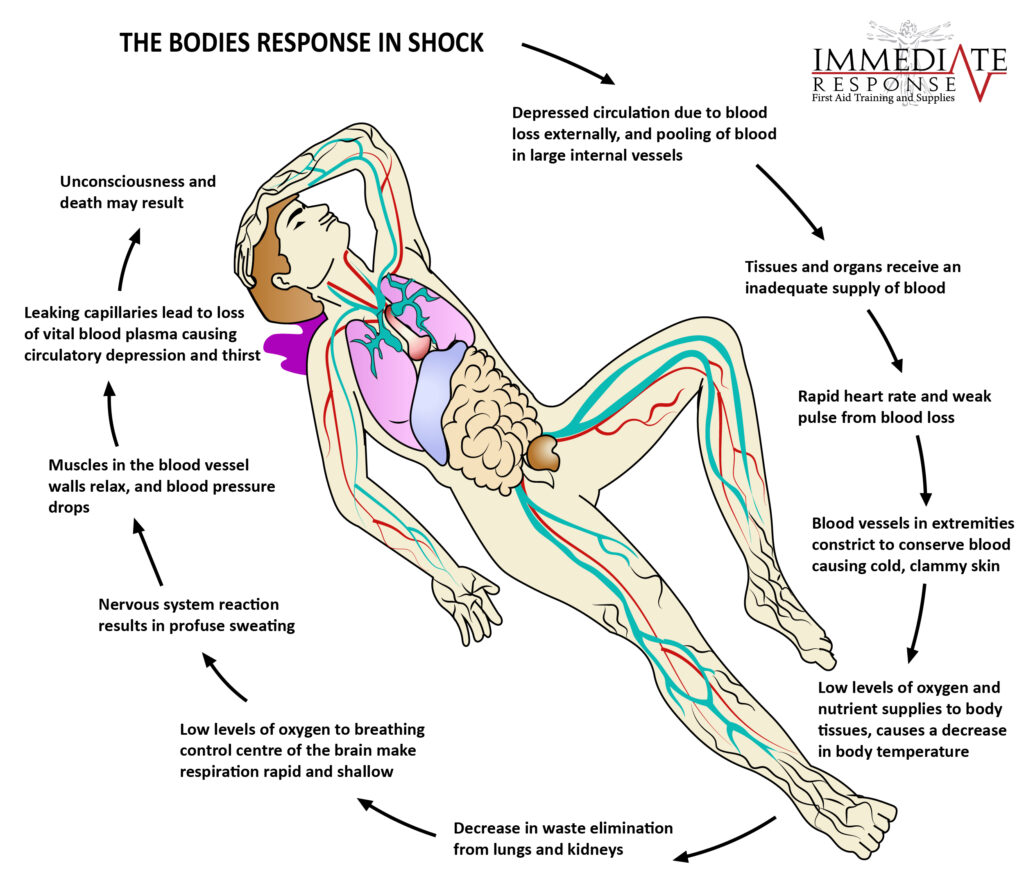
Shock occurs when the cardiovascular system fails to perfuse tissues adequately, resulting in widespread impairment of cellular metabolism. Because tissue perfusion can be disrupted by any factor that alters heart function, blood volume, or blood pressure, shock has many causes and various clinical presentations. Ultimately, however, shock from any cause progresses to organ failure and death, unless the causes are reversed or clinical intervention is successful.
Shock is classified by cause:
 Anaphylactic – a widespread hypersensitivity.
Anaphylactic – a widespread hypersensitivity.
 Cardiogenic – caused by heart failure.
Cardiogenic – caused by heart failure.
 Neurogenic – caused by alterations in vascular smooth muscle tone.
Neurogenic – caused by alterations in vascular smooth muscle tone.
 Septic – caused by infection.
Septic – caused by infection.
 Hypovolemic – caused by insufficient intravascular fluid volume.
Hypovolemic – caused by insufficient intravascular fluid volume.
 Allergic reactions.
Allergic reactions.
 Heart attack.
Heart attack.
 Brain or spinal injury.
Brain or spinal injury.
 Severe infection.
Severe infection.
 Severe bleeding, severe burns or scalds, severe diarrhoea and vomiting, severe sweating and dehydration.
Severe bleeding, severe burns or scalds, severe diarrhoea and vomiting, severe sweating and dehydration.

The casualty’s condition will depend on the severity of the underlying cause and may include.
 Rapid, weak pulse.
Rapid, weak pulse.
 Pale, cool, clammy skin (caused by the blood vessels constricting).
Pale, cool, clammy skin (caused by the blood vessels constricting).
 Weakness and/or dizziness.
Weakness and/or dizziness.
 Thirst.
Thirst.
 Nausea and/or vomiting.
Nausea and/or vomiting.
 Evidence of loss of body fluids, or high temperature if sepsis present.
Evidence of loss of body fluids, or high temperature if sepsis present.
 Confusion.
Confusion.
 Collapse leading to unconsciousness.
Collapse leading to unconsciousness.
 Slowing of the heart rate and respiration’s as the condition deteriorates, leading to death.
Slowing of the heart rate and respiration’s as the condition deteriorates, leading to death.

As a first aider, you can reduce some of the factors that lead to the shock process.
 Call 000 for an ambulance.
Call 000 for an ambulance. Reassure the casualty.
Reassure the casualty. Control any bleeding by applying pressure and elevation.
Control any bleeding by applying pressure and elevation.
 If conscious, lay the casualty down.
If conscious, lay the casualty down.
 If unconscious and breathing normally, place the casualty in the recovery position.
If unconscious and breathing normally, place the casualty in the recovery position.
 Conduct a secondary survey.
Conduct a secondary survey.
 Treat any other injuries.
Treat any other injuries.
 Maintain body temperature, but DO NOT overheat.
Maintain body temperature, but DO NOT overheat.
 Reassure the casualty.
Reassure the casualty.
 Loosen any restrictive clothing.
Loosen any restrictive clothing.
 Monitor vital signs (respirations, pulse rates and level of consciousness).
Monitor vital signs (respirations, pulse rates and level of consciousness).